Available in Audio Format:
Each of Canada’s ten provinces regulates gender medicine differently. This gives each province the ability to adapt to new evidence more quickly and respond to the demands of local citizens better than if health care were centralized with the federal government. But this also means that it is harder to understand all the nuances of each system and to collect data from across the country. Over the coming months, we will do our best to profile the data and policies on medical transitioning for minors in each province.
Newfoundland and Labrador is unique. It was the last province to join Canada (in 1949), has its own special time zone (30 minutes ahead of the rest of Atlantic Canada), and boasts the most distinctive accent in the country. The population of the entire province is smaller than the city of Hamilton, Surrey, or Quebec City. It is the least densely populated province in Canada, and just under half of the population resides in or around St. John’s.
Unfortunately, Newfoundland and Labrador is not unique when it comes to sex-denying medicine. While it does not perform sex-denying surgeries due to its size and lack of facilities, the province has not tapped the brakes on medical transitioning for minors.
Policy
Newfoundland and Labrador’s Medical Care Plan (MCP) generally covers the cost of puberty blockers and cross-sex hormones. The public health system also covers the cost of most sex-denying surgeries, but not all (e.g. facial feminization or voice pitch surgery).
Notably, all of the province’s policies and procedures relating to medical transitioning are based on the seventh version of WPATH’s Standards of Care (released in 2012) rather than the eighth version (released in 2022). The older edition notes that only 6-23% of cases of gender dysphoria in prepubertal children persisted into adulthood. Thus, “in most children, gender dysphoria will disappear before or early in puberty.”
Given this reality, the Standards of Care 7 are a bit more cautious about “gender-affirming care.” They recommend that clinicians working with gender dysphoric children and adolescents provide “supportive psychotherapy to assist children and adolescents with exploring their gender identity, alleviating distress related to their gender dysphoria.” But the Standards still support sex-denying procedures.
The seventh edition of the Standards of Care requires four criteria to be satisfied for clinicians to provide puberty blockers:
- The adolescent has demonstrated a long-lasting and intense pattern of gender nonconformity or gender dysphoria;
- Gender dysphoria emerged or worsened with the onset of puberty;
- Any co-existing psychological, medical, or social problems that could interfere with treatment have been addressed;
- The adolescent has given informed consent and, particularly when the adolescent has not reached the age of medical consent, the parents or other caretakers or guardians have consented to the treatment.
The Standards give no requirements for cross-sex hormones for minors specifically, though the following criteria are for hormone therapy in general:
- Persistent, well-documented gender dysphoria;
- Capacity to make a fully informed decision and to consent for treatment;
- Age of majority in a given country (if younger, follow the Standards of Care outlined in section VI [on children and youth]);
- If significant medical or mental health concerns are present, they must be reasonably well-controlled.
Curiously, although the third criterion refers to the section on children and youth, the section provides no further guidance on the prescription of cross-sex hormones to minors.
The Standards of Care 7 recommend that genital surgery not be performed prior to the age of majority, but suggests doing mastectomies earlier, “preferably after ample time of living in the desired gender role and after one year of testosterone treatment.” The requirements for surgery are the same as for cross-sex hormones, with the additional requirements of “12 continuous months of hormone therapy as appropriate to the patient’s gender goals (unless the patient has a medical contraindication or is otherwise unable or unwilling to take hormones)” for all genital surgeries and a further requirement of “12 continuous months of living in a gender role that is congruent with their gender identity” for genital reconstruction surgeries.
Thus, these requirements mandate no hard age limits on medical transitioning for minors, with the exception that bottom surgery is not recommended before the age of majority.
Providers
Trans Support NL, a non-profit organization that receives government funding, states that most gender-affirming care in the province is provided by a small group of providers that are mostly based in the St. John’s area. In response, the province is working to train primary care providers to provide gender-affirming care themselves. On its medical transitioning page, Trans Support NL encourages anyone seeking hormone replacement therapy to contact their family doctor.
However, there is one pediatric Gender Wellness Clinic at the Janeway Children’s Health and Rehabilitation Centre in St. John’s. The clinic serves children and youth under the age of 18 and is staffed by pediatric endocrinologists who prescribe puberty blockers and cross-sex hormones.
According to WPATH’s Standards of Care 7, only health care providers who meet “WPATH credentials” may provide surgical readiness assessments. Trans Support NL’s website lists four doctors who provide such assessments, though they note that the list is not exhaustive. Previously, the province had required a referral from the Centre for Addiction and Mental Health in Toronto for surgery.
The province does not perform most gender surgeries within the province. Most “top” surgeries are performed in New Brunswick, while most genital surgeries are performed at GRS Montreal.
Prevalence
In response to an access to information request, the government of Newfoundland and Labrador did not have any records detailing the number of minors who had received sex-denying interventions. The province was able to release data on the number of patients of all ages receiving puberty blockers or cross-sex hormones, but only for all underlying conditions (e.g. precocious puberty, breast or prostate cancer, menopause, or naturally low hormone levels in addition to a medical transition).
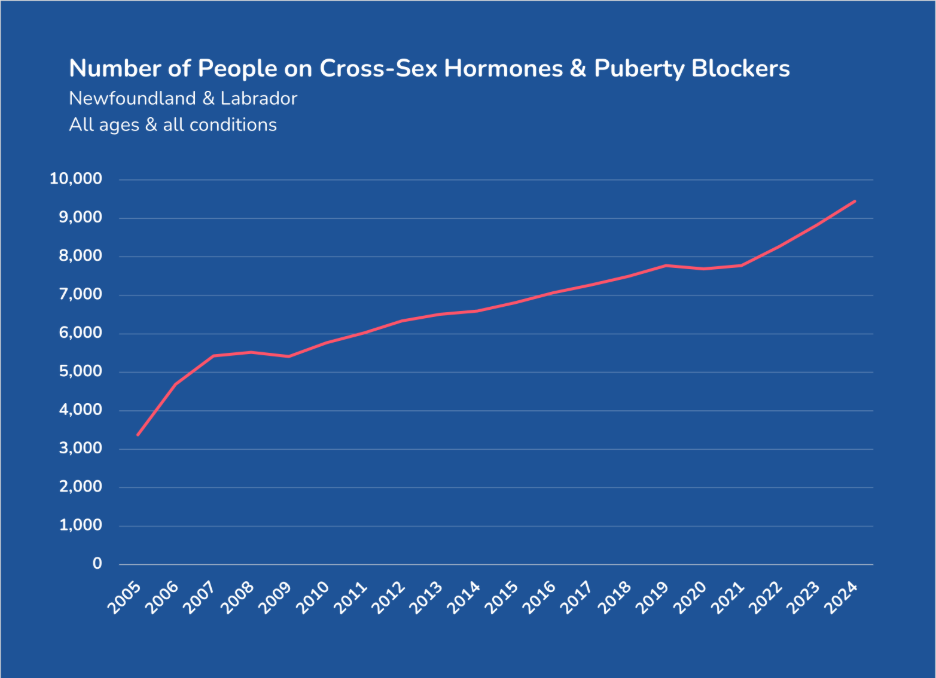
Given this level of aggregation, it is impossible to deduce the number of children, adolescents, or even adults who are hormonally transitioning. However, the use of these drugs has nearly tripled in two decades. More minors who are medically transitioning may be one factor driving that growth, but we cannot know for certain.
The only surgical data that Newfoundland & Labrador released was that it approved 169 sex-denying mastectomies between November 2019 and May 2022. Only 22 of these mastectomies were actually performed, however. One reason for this discrepancy could be that some women and girls reconsidered having their breasts permanently removed. The more likely reason is that, since no facility regularly performs these surgeries, most gender dysphoric women and girls have not (yet) travelled to have a mastectomy. The province provided no information regarding the age of the patients for whom mastectomies were approved or performed.
Conclusion
Although there are no legal restrictions on medical transitioning for minors in Newfoundland & Labrador, the province does rely on the older – and slightly more stringent – WPATH Standards of Care 7. These standards permit puberty blockers, cross-sex hormones, and top surgeries for minors, though they recommend bottom surgeries only after the age of majority. All of these procedures are eligible for public funding. No data on the number of minors who are medically transitioning is available.
And so, while Newfoundland & Labrador might be unique, they are not unique in their liberal provision of medical transitioning.
