In earlier articles, we highlighted how Sweden, Finland, and the United Kingdom are all hitting the brakes on medical transitioning for minors. More countries are following their lead.
Take Denmark. In 2018, 65% of youth seen by Denmark’s centralized gender service medically transitioned.1 Despite more warning signs popping up and new clinical guidelines being issued in other European countries – particularly in Denmark’s neighbours, Sweden and Finland – Denmark hasn’t officially changed its policies on medical transitioning. Yet, in 2022, only 6% of Danish youth referred to the gender service went on to medically transition, reflecting a new hesitancy among gender specialists in Denmark to refer children and adolescents for a medical transition. That decrease from 65% to 6% shows there is a quiet revolution against medically transitioning minors happening in Denmark.
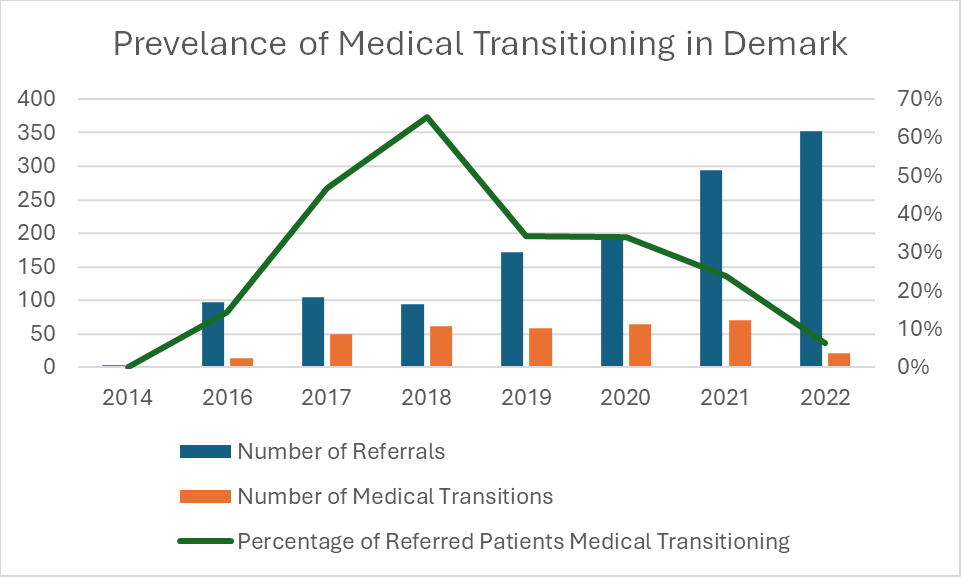
Denmark saw a steady rise in the number of youth coming to gender clinics with gender dysphoria, from 4 in 2014 to 352 in 2022. The percentage of these youth referred for medical transitioning has steadily fallen since 2018, though the absolute number of medical transitions only really fell significantly between 2021 (70) and 2022 (22). To take a page out of Shakespeare, something was rotten in the state of Denmark, but the Danes picked up the scent and have begun cleaning things up.
The medical establishment in Germany is calling on the government to replace its politically motivated approach to treating gender dysphoria with an evidence-based approach.
Or take Germany. Earlier this month, the 128th German Medical Assembly met. This association, self-described as “the central organisation in the system of medical self-administration in Germany,” is made up of delegates from the 17 state/provincial physician bodies. At their recent meeting, they passed a resolution calling on the German government to strictly limit medical transitioning for minors and for medical transitioning only to be permitted in controlled scientific studies.
The resolution says that “current medical evidence clearly and unambiguously states that puberty-blocking drugs (PB), opposite-sex hormone treatments (so-called cross-sex hormone administration [CSH]) and gender reassignment surgery (e.g. a mastectomy) do not improve GI/GD [gender incongruence/gender dysphoria] symptoms or mental health in minors with GI/GD. These are irreversible interventions in the human body in physiologically primarily healthy minors, who cannot give informed consent in the absence of evidence for such measures.”
Regrettably, the German government recently updated its official guidance in a manner that supports medical transitioning for minors. But the medical establishment in Germany is calling on the government to replace its politically motivated approach to treating gender dysphoria with an evidence-based approach.
Medical transitioning may be “one of the greatest ethical scandals in the history of medicine.”
Report from French Senators
Or take France. A group of French Senators initiated a report on medical transitioning for minors. The report, published earlier this year, claimed that the prevalence of medical transitioning may be “one of the greatest ethical scandals in the history of medicine.” Although the legislation hasn’t formally been introduced yet, several senators are working on a bill to prohibit medical transitioning for minors entirely in the country that they hope to introduce this summer.
And this is after the National Academy of Medicine in France released a statement urging medical practitioners to use the “greatest caution” when prescribing puberty blockers or cross-sex hormones, given “the side-effects such as the impact on growth, bone weakening, risk of sterility, emotional and intellectual consequences and, for girls, menopause-like symptoms.”
Actually, take psychiatric bodies across Europe. The European Society of Child and Adolescent Psychiatry (ESCAP) is an umbrella organization with societies in 36 member countries across Europe that helps its member societies discuss academic evidence in their fields, provide clinical guidance, and develop national health policies. At it’s recent meeting, it restated that an ethical pillar of medicine is to do no harm, a commitment featured in the Hippocratic Oath.
Conversely, the goal of medical interventions is beneficence, to do good. Therefore, any medical intervention must be based on sound science supporting its efficacy to do good and not to do harm, to restore or preserve mental and physical health rather than impairing health. Given the lack of evidence supporting medical transitioning, ESCAP calls on health care providers “not to promote experimental and unnecessarily invasive treatments with unproven psycho-social effects and, therefore, to adhere to the ‘primum non nocere’ (first, do no harm) principle.”
As we can see from all of these examples, there is a growing movement in more and more countries to stop medical transitioning for minors.
Will Canada finally examine the evidence and follow suit?
Last week, Dr. Hilary Cass, chair of the independent review of Gender Identity Services for children and young people, released her final report. The review was spurred by widespread controversy over the Gender Identity Development Service at the country’s Tavistock clinic. While other jurisdictions – notably Finland and Sweden – had done comprehensive reviews of their pediatric transitioning programs, their conclusions received little press in Canada and the English-speaking world.
This Cass Review is the most important document on the topic of medical transitioning for minors in the English-speaking world. And its findings and recommendations are striking.
Medical Transitioning in the UK
The review highlights how the UK’s gender identity services went about their work with an utter disregard for the scientific method and medical caution. The Gender Identity Development Service (GIDS) was established in 1989 and, for several decades, saw very few patients. Most of these patients were pre-pubescent boys with acute gender dysphoria. The service usually provided counselling, not medical treatments. In 2011, following a novel approach to treating gender dysphoria pioneered in the Netherlands, GIDS decided to begin prescribing puberty blockers to children as a part of a research program – a medical trial. Essentially, the Gender Identity Development Service didn’t know whether prescribing puberty blockers to try to give children time to explore their gender identity would be better than just counselling, so they decided to do the rational thing to find out: start a medical trial.
But they never finished this early intervention study. In fact, GIDS didn’t even collect the data they were supposed to. Instead, they ploughed ahead with prescribing puberty blockers and then cross-sex hormones to more and more children and adolescents without ever actually learning whether this was in their young patients’ best interest. In essence, they expanded their medical trial to thousands of children without looking back to see whether the treatment was working.
When this came to light, the National Health Service commissioned Dr. Hilary Cass to review the entire model of gender care in the UK. GIDS dug through its patient consultation notes and follow-up with patients to find the data needed to evaluate the Service’s medical transitioning program. When the results were finally published in 2021, they found that “there were no statistically significant changes reviewed in gender dysphoria or mental health outcome measures whilst on puberty blockers.”
“…there were no statistically significant changes reviewed in gender dysphoria or mental health outcome measures whilst on puberty blockers.” – Cass Report
Examining All of the Evidence
But the Cass Review didn’t just want to see how children had fared under the care of GIDS. Cass commissioned six independent systematic reviews of all available evidence of medical transitioning for minors to see if medical transitioning could ever reliably improve health and well-being. Systematic reviews are the highest quality academic evidence available because they collect all the studies done on an issue and combine, compare, and analyze their results. This allows researchers to learn from other time periods, other places, and other methods of study.
These systematic reviews all reached the same conclusion: there is no high-quality evidence to support medical transitioning for minors.
For example, the University of York’s systematic review concluded:
- “there is insufficient and/or inconsistent evidence about the effects of puberty suppression on psychological or psychosocial health” (176);
- “[there is] no evidence that puberty blockers improve body image or dysphoria, and very limited evidence for positive mental health outcomes” (p. 179); and
- “the evidence for the indicated uses of puberty blockers and masculinising/feminising hormones in adolescents are unproven and benefits/harms are unknown” (194).
Medical transitioning for minors was a failure. The overview of the review’s key findings states that “for most young people, a medical pathway will not be the best way to manage their gender-related distress.” Puberty blockers and cross-sex hormones would not be offered to minors under the age of 16. Even for adolescents over age 16, the Review recommends “extreme caution.”
These systematic reviews all reached the same conclusion: there is no high-quality evidence to support medical transitioning for minors.
The Cass review also found that the World Professional Association for Transgender Health (WPATH)’s Standards of Care – the clinical guidelines predominantly followed in Canada – were not based on high quality evidence. In fact, WPATH’s Standards of Care didn’t even bother to reference its own systematic review of the literature on medical transitioning but claimed instead that a “systematic review regarding outcomes of treatment in adolescents is not possible” (131). But it was possible. The Cass Review produced six. WPATH completed one but ignored it.
It appears that the commitment of WPATH and other bodies to “gender affirming care” was ideological, not evidence-based. The Cass Review found that few medical bodies around the world were willing to admit the lack of evidence to support medical transitioning.
Evidence is Evidence, No Matter What Country You’re In
Following the publication of the Cass Review, the CBC solicited responses from Canadian doctors on the findings of the Review. These doctors and the Canadian Pediatric Society – who have not bothered to publicly assess all the available evidence in systematic reviews or craft standards of care specific to Canada – think they know the evidence on medical transitioning for minors better. These Canadian bodies continue to stand by the practice of medical transitioning for minors, despite the lack of high-quality evidence supporting the practice and even while many countries, and the province of Alberta, are restricting the availability of puberty blockers and cross-sex hormones to minors.
“…if no high quality evidence for medical transitioning is established in the coming years – that medical transitioning for minors is the great medical scandal of our time.” – Dr. J. Edward Les
Of course, Canadian doctors are not a monolithic group. Some doctors, such as Dr. J. Edward Les, have decried Canada’s direction on the issue. Dr. Les points out that there have been numerous examples in the last hundred years alone of medical consensuses leading to horrible practices that incapacitated, addicted, or even killed thousands of people. He’s afraid – rightly, if no high quality evidence for medical transitioning is established in the coming years – that medical transitioning for minors is the great medical scandal of our time.
That’s why Let Kids Be exists. As a country, we need to be humble when mistakes have been made and be courageous to correct our mistakes. Thus far, only the political arm in Alberta has been humble and courageous enough to ban medical transitioning for minors. Other provincial governments and our medical establishments need to follow suit.
Will you take action and help us make this a reality?
“Would you rather have a live son or a dead daughter?”
This is the choice that gender ideology advocates often give to parents with a gender dysphoric child. It’s a bit ironic that they reject the gender binary but phrase this as a stark binary choice. They claim that because children and adolescents who identify as transgender are far more likely to contemplate, attempt, and commit suicide, the only way to save them from suicide is medical transition and full acceptance by everyone as the opposite sex.
That’s the claim. But what’s the evidence?
Almost every study indicates that kids who identify as transgender are more likely to contemplate, attempt, and commit suicide. Bauer et al. document that 22-43% of people who identity as transgender in Canada, Europe, and the United States have attempted suicide; 35% of Ontarians who identify as transgender had seriously considered suicide and 11% had actually attempted suicide in the past year alone.1 Considering that only 3.7% of all Canadians had ever seriously considered suicide and only 0.6% had attempted suicide in the past year, Ontarians who identify as transgender were 9.5 times more likely to seriously consider suicide and 18 times more likely to attempt suicide than the average Canadian in the past year.
Would you rather have a live son or a dead daughter?
Few studies examining the outcomes of medical transition take a longitudinal approach, which would mean collecting information over a long period of time rather than just shortly after transition. Dhejne et al. is the best study in this regard, studying 324 people who underwent a surgical transition between 1973-2003 and following their outcomes for up to 30 years.2 Overall mortality (e.g. the risk of dying from any cause) was statistically the same for the first 10 years after transition for people who underwent a surgical transition compared to a control group from the transgender population. But the mortality rate among those who had surgically transitioned significantly increased after 10 years. Those who had surgically transitioned were 2.9 times more likely to die from any cause, 19 times more likely to die by suicide, and 7.6 times more likely to consider suicide compared to the general population.
Many advocates and scholars explain this risk of suicidality through minority stress theory. This theory posits that stigma, prejudice, and discrimination against people experiencing gender dysphoria create a hostile and stressful social environment that causes them to consider suicide. However, Bränström et al. conclude that minority stress is a relatively minor factor behind these poor outcomes, finding that only 13-15% of suicidal ideation and attempts are attributable to minority stress.3
Little attention has been paid to the possibility that gender dysphoria itself (and any comorbid conditions) directly contributes to suicidality. If our gender is determined by our biology rather than by our feelings, then it would be unsurprising that these correlations or even causations exist. Medical and surgical transitioning won’t fix these problems. If anything, they are likely to make them worse in the long-term.
Medical and surgical transitioning won’t fix these problems. If anything, they are likely to make them worse in the long-term.
And that’s what some studies show.
Even though people who identify as transgender are at a much higher risk of suicide than the general population, medical transitioning does not lower this risk. Dallas et al. analyzed the outcomes of Californians who underwent a surgical transition (a vaginoplasty for males attempting to become females and a phalloplasty for females attempting to become males) from 2012-2018.4 Among those who had a phalloplasty, the rate of suicide attempts did not change after the procedure, even though the phalloplasty was supposed to affirm their new gender identity and decrease their risk of suicide. For those who had a vaginoplasty, the suicide rate doubled after surgery.
Many studies claim that medical transitioning reduces suicidality, suicide attempts, and suicide death. But virtually all of these studies suffer from the same methodological weaknesses: observational analyses (rather than randomized trials), short-term time frames, small sample sizes, high non-response or drop-out rates, and the presence of confounding variables (rather than clear causal links), all of which make them low-quality studies.
This conclusion was affirmed in a recent systematic review, The Impact of Gender-affirming Surgeries on Suicide-Related Outcomes, by Marques et al. in 2023.5 Systematic reviews are some of the most valuable academic sources because they find and assess all of the academic studies on a topic. Marques et al. found 11 studies on the impact of medical transitioning on suicidality. They found “a wide scope of results” and concluded that “GAS’ [gender-affirming surgeries] influence on suicide deaths cannot be drawn due to the low quantity and quality of evidence.”
Furthermore, a Finnish study published this year by Ruuska et al. corrected many problems with earlier studies (e.g. had matched controls, long-term data, a large sample size, a full response rate, and analyzed confounding variables) found that the increased risk of suicide among young people referred to a gender identity clinic disappeared once psychiatric treatment was accounted for.6 In other words, the high rate of suicide among young people with gender dysphoria was due to other psychiatric conditions, not gender dysphoria.
The claim that medical transitioning is necessary to prevent suicide is not supported by high quality evidence.
In summary, the claim that medical transitioning is necessary to prevent suicide is not supported by high quality evidence. While people suffering from gender dysphoria may be at a higher risk of suicide than the average person, it is likely that other mental health conditions, not the gender dysphoria per se, are causing this suicidality.
Instead of medical transitioning, kids need mental health supports. In other words, children identifying as transgender need the help of loving parents and patient counsellors to live healthy and happy lives in the bodies they were born with.
- Greta R. Bauer et al., “Intervenable Factors Associated with Suicide Risk in Transgender Persons: A Respondent Driven Sampling Study in Ontario, Canada,” BMC Public Health 15, no. 1 (June 2, 2015): 525, https://doi.org/10.1186/s12889-015-1867-2. ↩︎
- Cecilia Dhejne et al., “Long-Term Follow-Up of Transsexual Persons Undergoing Sex Reassignment Surgery: Cohort Study in Sweden,” PLOS ONE 6, no. 2 (February 22, 2011): e16885, https://doi.org/10.1371/journal.pone.0016885. ↩︎
- Richard Bränström et al., “Transgender-Based Disparities in Suicidality: A Population-Based Study of Key Predictions from Four Theoretical Models,” Suicide and Life-Threatening Behavior 52, no. 3 (2022): 401–12, https://doi.org/10.1111/sltb.12830.5. ↩︎
- Kai Dallas et al., “Mp04-20 Rates of Psychiatric Emergencies before and after Gender Affirming Surgery,” Journal of Urology 206, no. Supplement 3 (September 2021): e74–75, https://doi.org/10.1097/JU.0000000000001971.20. ↩︎
- Inês Rafael Marques et al., “The Impact of Gender-Affirming Surgeries on Suicide-Related Outcomes: A Systematic Review,” Journal of Psychosexual Health 5, no. 3 (July 1, 2023): 134–44, https://doi.org/10.1177/26318318231189836. ↩︎
- Sami-Matti Ruuska et al., “All-Cause and Suicide Mortalities among Adolescents and Young Adults Who Contacted Specialised Gender Identity Services in Finland in 1996–2019: A Register Study,” BMJ Ment Health 27, no. 1 (January 1, 2024), https://doi.org/10.1136/bmjment-2023-300940. ↩︎
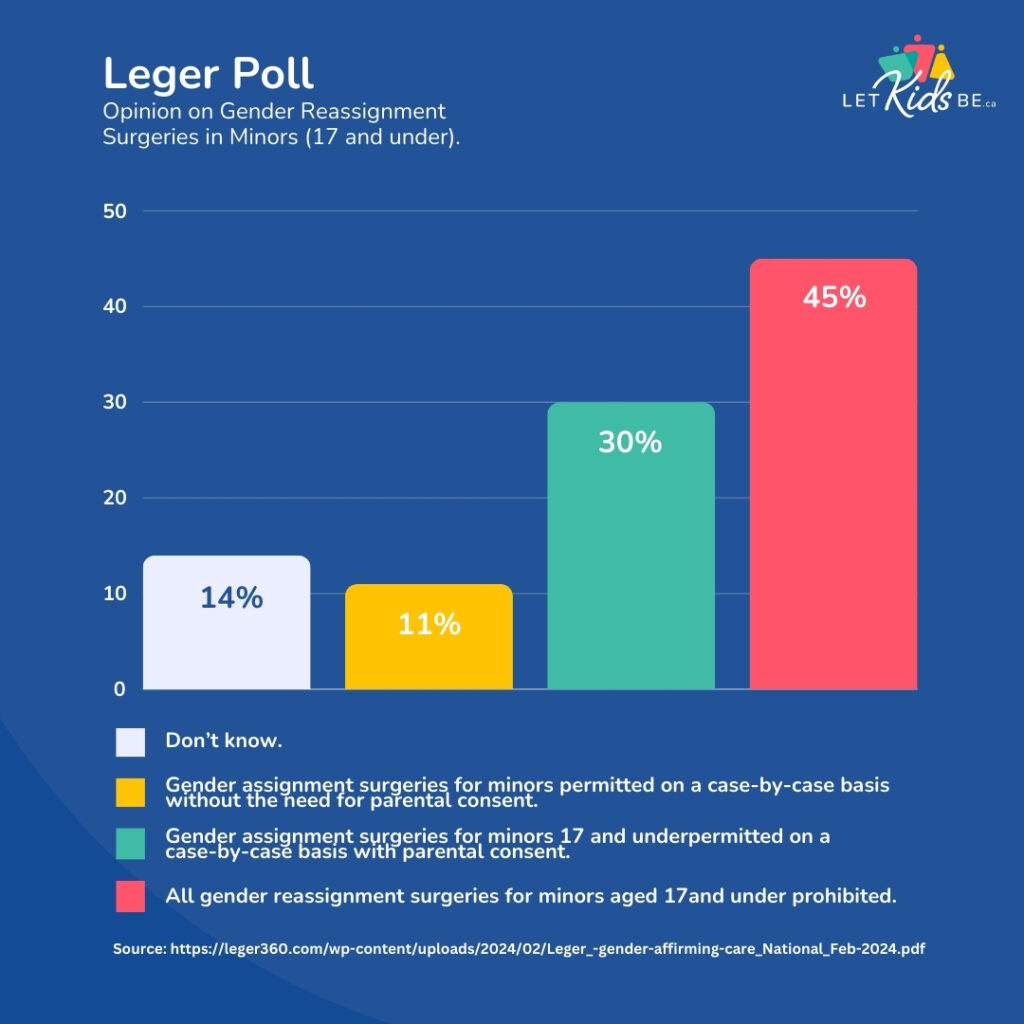
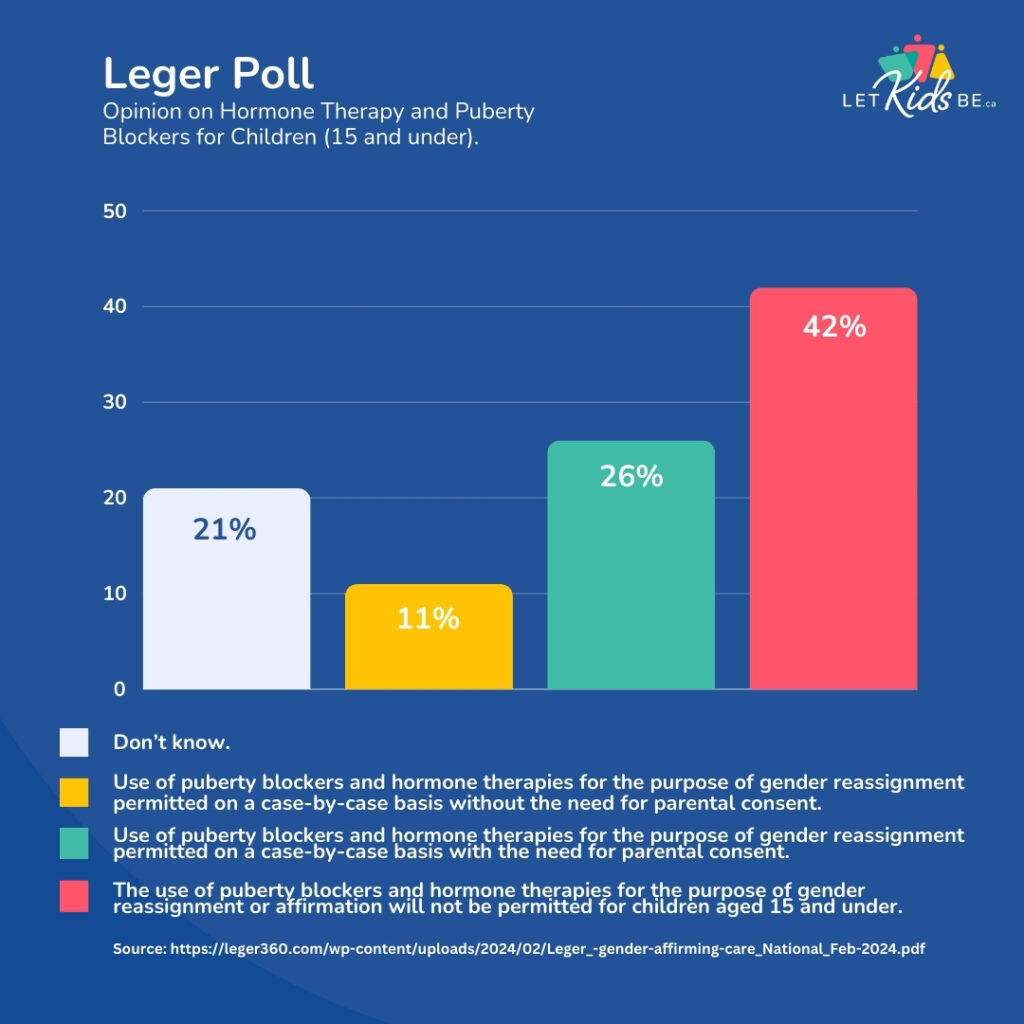
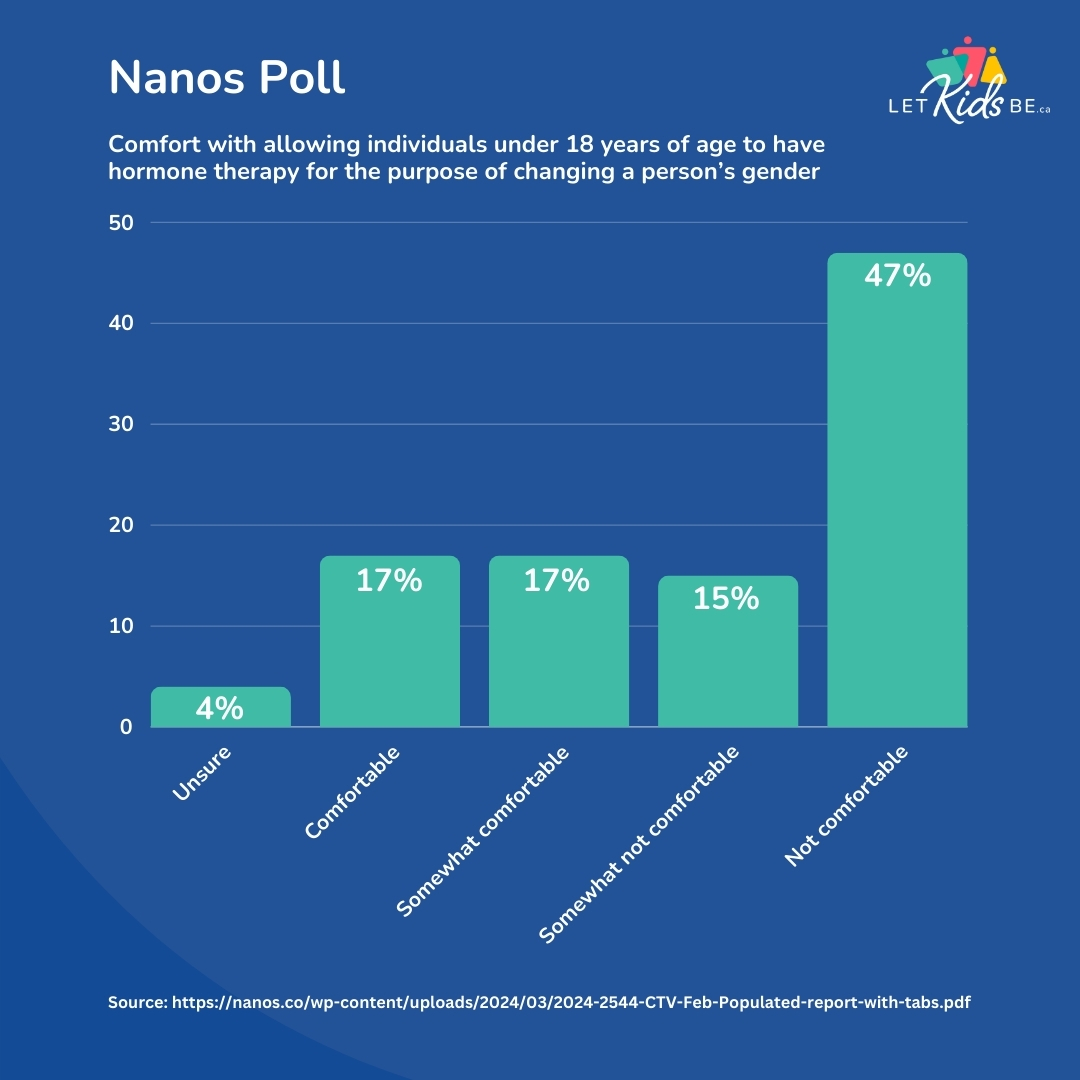
Within the last month, two reputable polling firms – Leger and Nanos – have asked Canadians their opinions on various transgender policies. And their position is clear.
According to the Leger poll, 45% of Canadians think that all gender reassignment surgeries for minors aged 17 and under should be prohibited, 30% think that such surgeries should be legal for minors on a case-by-case basis with parental consent, and only 11% say that such surgeries should be legal without parental consent.
A similar number of Canadians – 42% – would also ban the use of puberty blockers and cross-sex hormones for minors aged 15 and under, with 26% opining that such that such interventions be legal on a case-by-case basis with parental consent and only 11% thinking that they can be prescribed without the need for parental consent. Those figures drop to 35% in favour of banning hormonal interventions, 24% in favour of allowing them with parental consent, and 23% allowing them without parental consent for youth aged 16-17.
Nanos found similar numbers. Forty-seven percent of Canadians are not comfortable with allowing minors aged 17 and under to receive puberty blockers or cross-sex hormones. An additional 15% are somewhat uncomfortable with this intervention. Only 17% are somewhat comfortable and another 17% are fully comfortable with puberty blockers and cross-sex hormones for minors.
Three things stand out from these polls.
First, a plurality of Canadians is clearly uncomfortable with medical transitioning for minors and want them banned. Almost half of Canadians (45% in the Leger poll and 47% in the Nanos poll) espouse this position. Canadians who value the bodily integrity of children outnumber the medical transitioning proponents by three or four to one.
Second, age matters. While neither poll asked Canadians view on medical transitioning for adults, Canadians seem to have various opinions on mature minors receiving puberty blockers and cross-sex hormones. Leger found that 42% of Canadians support banning these hormonal interventions for minors aged 15 and below, but that number drops to 35% when those interventions are offered for youth aged 16-17.
Third, parental consent matters. The Nanos poll reveals that 34% of Canadians are somewhat comfortable or somewhat uncomfortable with medical transitioning for minors, but their polling doesn’t get at the reason why Canadians are uncomfortable with idea. The Leger poll provides some context, showing that parental consent is a big deal in the minds of most Canadians, with approximately a third of Canadians viewing the issue through the lens of parental rights.
Time to turn public opinion into public action and public policy.
These polls provide further support for politicians to heed the call to ban medical transitioning for minors. Ultimately, it isn’t the voice of the majority that should dictate public policy. Evidence and facts should. We already know that kids can’t consent to these procedures, that these interventions have a long list of negative side effects, and they fundamentally don’t change a person’s sex. So, the evidence and philosophy is already there.
Now public opinion is there too.
Time to turn public opinion into public action and public policy. Here’s two things you can do:
1. Send an email using ARPA Canada’s EasyMail tool asking your MPP or MLA to stop the medical transition of minors.
2. If you’re in British Columbia or Ontario, print off some petition sheets, get them signed and send off to the address at the bottom of the sheet.
The goal of Let Kids Be is to ban medical and surgical transitioning for minors. Many Canadians think that this is a radical proposal. That it is an attack on trans rights. But is it?
In short, no. Many developed jurisdictions, both progressive and conservative alike, have begun to realize the problems presented in previous articles and are greatly restricting medical and surgical transitioning.
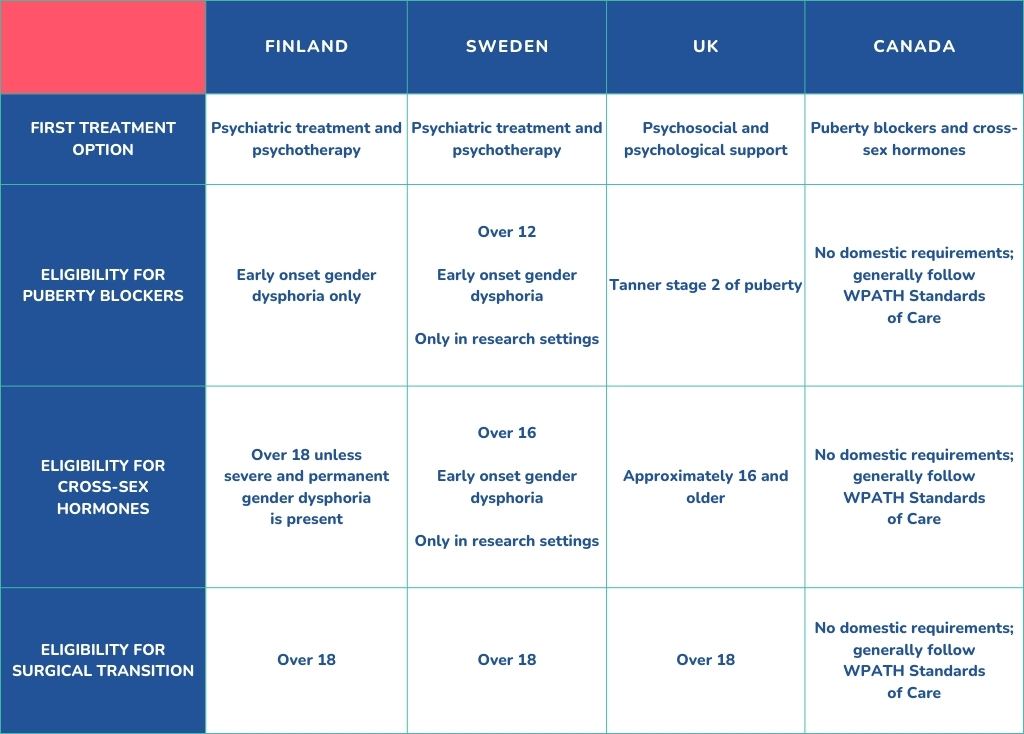
In 2020, the Finnish Health Authority broke with the prevailing gender-affirming model of care which rushes children and adolescents into medical and surgical treatments. Instead, psychiatric treatment and psychotherapy are once again the first steps prescribed to address gender dysphoria. Cross-sex hormones are generally available only to persons over the age of 18. Surgical treatments are not considered treatment methods for dysphoria in minors. The Finnish Health Authority also warns against any irreversible gender-affirming interventions for those below the age of 25, due to a lack of neurological maturity.1
In Finland, surgical treatments are not considered treatment methods for dysphoria in minors.
In 2021, Astrid Lindgren Children’s hospital in Sweden decided not to provide puberty blockers or cross-sex hormones to persons under the age of 16. For those aged 16-18, hormonal treatments would only be offered within clinical trials.2
In 2022, the Swedish National Board of Health and Welfare reformed their standards of care across the board, following Finland’s approach of making psychological and psychiatric care the first treatment option for all minors. They will allow cross-sex hormones only for people with early-onset gender dysphoria and at a minimum age of 16.3
In 2022, the United Kingdom’s sole child gender identity clinic in Tavistock was closed in favour of a decentralized regional hub model following the release of the Cass Report, an interim report that studied the treatment of gender dysphoria in the United Kingdom. Although the report made no definitive recommendations, it did find that “an unquestioning affirmative approach is at odds with the standard process of clinical assessment and diagnosis that they have been trained to undertake in all other clinical encounters” and that greater safeguards, such as a formal diagnosis of gender dysphoria prior to hormonal treatment, was necessary.4
In 2023, the UK’s National Health Service issued new interim guidance, reminding clinicians that “this may be a transient phase, particularly for pre-pubertal children,” that a “significant proportion of children and young people who are concerned about, or distressed by, issues of gender dysphoria experience coexisting mental health, neuro-developmental and/or personal, family or social complexities in their lives,” and that there are “risks of an inappropriate gender transition.” The primary intervention is now psychosocial and psychological support.5
A growing refrain from these national reviews is that there is a lack of evidence to support these medical and surgical interventions, particularly in the long-term.
In 2022, the National Academy of Medicine in France released a statement urging medical practitioners to use the “greatest caution” when prescribing puberty blockers or cross-sex hormones, given “the side-effects such as the impact on growth, bone weakening, risk of sterility, emotional and intellectual consequences and, for girls, menopause-like symptoms.”6
In 2023, the Norwegian Healthcare Investigation Board also found their national professional guidelines to be too loose and overly biased in favour of hormonal and surgical interventions. Like the United Kingdom in the Cass Report, Norway will be re-drafting its guidance on gender-affirming care.7
Finally, a growing number of American states (21 as of December 2023) have introduced, debated, and passed laws that ban the provision of puberty blockers, cross-sex hormones, and/or gender reassignment surgery to minors.8
A growing refrain from these national reviews is that there is a lack of evidence to support these medical and surgical interventions, particularly in the long-term. It is clear that these interventions are still experimental at best, with a growing body of evidence suggesting they do profound harm with no benefit to the patient.
Canada must follow suit.
Canada’s current gender-affirming approach to gender dysphoria must be abandoned in favour of body-affirming care. If there is a perceived dysphoria between a person’s biological sex and their gender identity, health care practitioners should understand that trying to change biological sex is far more risky, difficult, and invasive than psychiatric treatment and psychotherapy that seek to change self-perception. Fundamentally, biological sex cannot change but the self-perception of the psychological, social, and cultural aspects of being male and female can change. This is why psychiatric treatment and psychotherapy are becoming the first treatment method of choice for countries such as Finland and Sweden.
Unfortunately, pursuing these alternatives to gender-affirming care is risky for anyone within or even outside of health care due to various federal and provincial bans on conversion therapy. The poorly written federal conversion therapy legislation bans “any practice, treatment or service designed to… change or repress a person’s gender identity to cisgender or… change, repress, or reduce a person’s gender expression so that it conforms to the sex assigned to the person at birth.”9 This legislation effectively shuts the door to body-affirming care and leaves gender-affirming care as the only legally permissible treatment for gender dysphoria.
Fundamentally, biological sex cannot change but the self-perception of the psychological, social, and cultural aspects of being male and female can change.
Addressing gender dysphoria must be a holistic, multifaceted process. Gender dysphoria – the psychological distress caused by a perceived incongruence between one’s biological sex and perceived gender – must be alleviated. Any comorbidities must be diagnosed and treated. The religious and cultural beliefs of the patient as well as their parents must be respected. The influence of peer groups on gender identity must be understood and countered, if required. The negative impacts of social media and web consumption must also be counteracted.
Gender dysphoria is not something that is easily solved by hormones or surgery. It is far more complicated than that.10
While there are all sorts of policies that our government can implement in Canada in response to this issue, the most urgent one is to stop the practice associated with the greatest harm: medical and surgical transitioning for minors. We call upon Canada’s provincial governments to prohibit the provision of puberty blockers, cross-sex hormones, and gender reassignment surgeries for minors.
Will you join us?
- Society for Evidence Based Gender Medicine, “One Year Since Finland Broke with WPATH Standards of Care,” July 2, 2021, https://segm.org/Finland_deviates_from_WPATH_prioritizing_psychotherapy_no_surgery_for_minors. ↩︎
- Society for Evidence Based Gender Medicine, “Sweden’s Karolinska Ends All Use of Puberty Blockers and Cross-Sex Hormones for Minors Outside of Clinical Studies,” May 5, 2021, https://segm.org/Sweden_ends_use_of_Dutch_protocol. ↩︎
- Society for Evidence Based Gender Medicine, “Summary of Key Recommendations from the Swedish National Board of Health and Welfare,” February 27, 2022, https://segm.org/segm-summary-sweden-prioritizes-therapy-curbs-hormones-for-gender-dysphoric-youth. ↩︎
- Cass, “Interim Report – Cass Review.” ↩︎
- NHS England, “Interim Specialist Service for Children and Young People with Gender Incongruence,” June 9, 2023, https://www.england.nhs.uk/wp-content/uploads/2023/06/Interim-service-specification-for-Specialist-Gender-Incongruence-Services-for-Children-and-Young-People.pdf. ↩︎
- French National Academy of Medicine, “Medicine and Gender Transidentity in Children and Adolescents,” February 25, 2022, https://www.academie-medecine.fr/la-medecine-face-a-la-transidentite-de-genre-chez-les-enfants-et-les-adolescents/?lang=en. ↩︎
- National Commission of Inquiry for the Health and Care Service, “Patient Safety for Children and Young People with Gender Incongruence,” Ukom, March 9, 2023, https://ukom.no/rapporter/pasientsikkerhet-for-barn-og-unge-med-kjonnsinkongruens/sammendrag. ↩︎
- Although we profoundly disagree with their framing of this issue, the Human Rights Campaign has an informative map of which states have banned some form of gender-affirming care that is regularly updated: https://www.hrc.org/resources/attacks-on-gender-affirming-care-by-state-map ↩︎
- Section 320.101, Criminal Code of Canada. ↩︎
- Bailey and Blanchard, “Gender Dysphoria Is Not One Thing.” ↩︎
In the last 10-15 years, we have all anecdotally sensed a rise of the transgender movement, with more and more people identifying as transgender, more media outlets talking about gender identity in their stories, and more politicians pledging their support for the LGBTQ2S+ movement. But what does the data say? How many people, and specifically children, are identifying as transgender and seeking a medical and then a surgical transition here in Canada?
The answer takes us down a windy road.
International Numbers
The beginning of the answer lies in the United Kingdom. For decades, the Tavistock clinic in the United Kingdom was the lone clinic in the country that specialized in treating children with gender dysphoria. The clinic initially began under the condition that their work with gender dysphoric children be part of a research study that would analyze the results of treating gender dysphoria in children. In other words, they were supposed to collect the data on the number of referrals to the clinic.
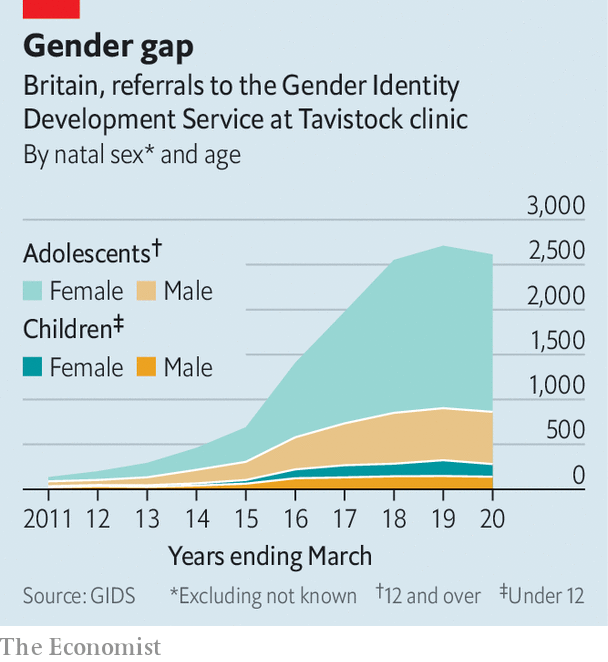
Image source: The Economist
But for years, they didn’t. Only after the Tavistock clinic imploded in public scandal and legal proceedings did the clinic go back through its archives and begin assembling the data required to start reviewing its work.
The Economist magazine was one of the first mainstream institutions to publish some of this data. Their data showed a 30-fold increase in referrals to Tavistock over the course of a decade, empirically validating what everyone was witnessing around them.
The collapse in the Tavistock clinic initially led to a leveling off in the number of minors referred to a gender clinic throughout the United Kingdom, leading some commentators to think that the country had begun to course correct in their treatment of gender dysphoria and that the exponential rise in the number of referrals had reached a ceiling.
That proved not to be the case. A few years later, the Society for Evidence-Based Medicine revealed that the number of referrals to gender clinics continued to rise rapidly in the network of gender clinics that opened across the country after Tavistock’s demise was in place. The rise continued and was mirrored in data from other countries such as Sweden.
So, the numbers of kids being referred to gender clinics for gender dysphoria has clearly skyrocketed in recent years in some Western jurisdictions. What about here in Canada?
Canadian Numbers
Collecting data on the number of minors diagnosed with gender dysphoria or going through a medical and surgical transition is difficult. Each province has their own health care system, and each province generally doesn’t publish their health service data. Thus, there has been a dearth of information on this issue in Canada.
For years, the best source of information was a study entitled “Trans Youth Can!” The study included participation from ten gender clinics across Canada (BC Children’s Hospital Gender Clinic in Vancouver, Alberta Children’s Hospital METTA Clinic in Calgary, Stollery Children’s Transgender Clinic in Edmonton, GDAAY Clinic in Winnipeg, LHSC Children’s Hospital Gender Pathways Service in London, McMaster Children’s Hospital Adolescent Medicine Clinic in Hamilton, SickKids Hospital Gender Clinic in Toronto, CHEO Diversity Clinic in Ottawa, Centre Meraki in Montreal, and IWK Health Centre Transgender Clinic in Halifax). Presentation slides from the study listed the number of referrals to specialist clinics for puberty blockers or gender-affirming hormones for nine Canadian clinics. No other information about these numbers accompany the graph, making it difficult to explore this data further.
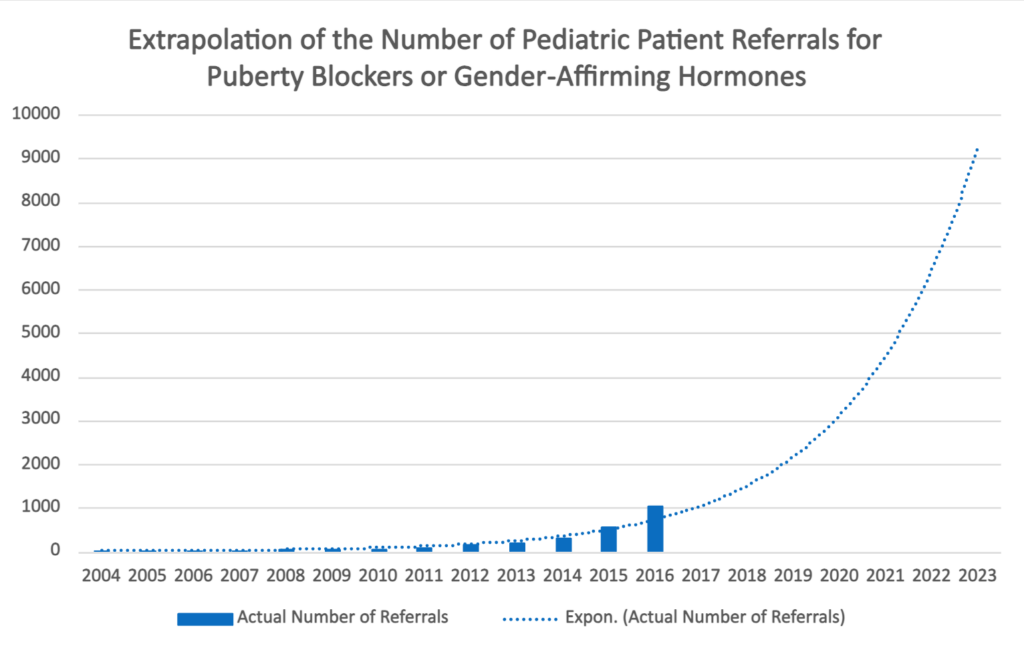
Since 2016, the Trans Youth Can! study has not updated its figures for the number of referrals to gender clinics for puberty blockers or cross-sex hormones nor has there been another aggregation of referrals to gender clinics in other studies or data sources. However, extrapolating the data pattern presented in this Trans Youth Can! study would suggest that thousands of children are being referred for a medical transition. While it is unlikely that this trend continued without interruption through the COVID-19 pandemic and a growing number of figures urging caution when proceeding to a medical transition, this estimation can give us some idea of the magnitude of this issue.
Thankfully, one organization, the Canadian Institute for Health Information (CIHI), is dedicated to aggregating provincial-level health data and making it available for policy-makers, journalists, and citizens. Our team has requested data from CIHI regarding the number of minors who have medically and surgically transitioned.
Unfortunately, CIHI wasn’t able to provide us data on the number of referrals to gender clinics or puberty blockers or cross-sex hormones prescriptions. CIHI collects data primarily from public drug programs and claims that most puberty blockers and cross-sex hormone prescriptions are funded through private drug plans, and so they did not have the information available.
However, CIHI was able to release some data on the number of surgical transitions for minors. Thankfully, although there are no hard age requirements to go through a surgical transition in Canada, CIHI reports that there were less than five “bottom” surgeries (outside of Quebec, at least) between 2018 and 2023. While the fact that these procedures are legally allowed for minors is troubling, they seem to be extremely rare in Canada.
That premise does not hold true when it comes to “top” surgeries – mastectomies, the surgical removal of breasts. In the last five years, exactly 300 underage girls (outside of Quebec) had their breasts surgically removed to try to alleviate their gender dysphoria. That’s the equivalent of one every six days. According to reporting by Sharon Kirkey of the National Post, the youngest recipient of such as double mastectomy was 14. While we would like to get data on these surgical transitioning procedures prior to 2018, CIHI only disaggregated mastectomies for the purpose of transitioning from mastectomies for other reasons (e.g. breast cancer or cosmetic changes) starting in 2018.
And these numbers of “top” and “bottom” surgeries for minors doesn’t mean that the kids who did not receive these procedures are out of the woods. Many of them will choose or be encouraged to undergo these procedures as they enter adulthood.
Conclusion
As it stands right now, while we know that there are very few cases of “bottom” surgery on minors in Canada, dozens of “top” surgeries happen every year, and there are likely thousands of instances of minors being prescribed puberty blockers and/or cross-sex hormones as the default treatment for gender dysphoria. Every instance is a tragedy, the culmination of decades of misunderstanding about what human beings fundamentally are and what the purpose of medicine is.
Instead of medically transitioning children and surgically removing the healthy breasts of girls, we need to let kids be. Will you help us reach our provincial governments with the message that we need to end medical transitions for minors? Send an email to your provincial representative today!
In our previous articles, we talked about how the current model of medical and surgical transitioning is built on faulty anthropology. It misdiagnoses the fundamental problem with gender dysphoria and so provides the wrong solution, and it doesn’t actually successfully address gender dysphoria.
But all of these truths apply to people of any age. And so, why is the Let Kids Be campaign focused just on minors instead of all people with gender dysphoria?
The reason for our focus on minors is centered on consent. In Canada, we prize freedom and consent highly. We generally don’t want to place many restrictions on people, especially on what they do or don’t do with their own body. For better or worse, we trust rational people to make decisions for themselves, even if that allows them to make what most other people would consider the wrong decision.
The caveat to this is that people must be rational or mature enough to make these decisions. Children and adolescents, though, are still in the stage of life where their brain is developing. All across Canada there are minimum ages (e.g. 18 or 19) for a variety of relatively trivial matters (e.g. to change your legal name, buy a lottery ticket, donate blood, watch an R-rated movie, or adopt a pet from the SPCA) as well as more consequential matters (e.g. to marry, join the armed forces, buy cigarettes, or consume alcohol).1 Governments restrict these activities because they realize certain risks and their ensuing obligations are only appropriate for certain ages.
The issue with medical and surgical transitioning is that there are no age requirements specified in the World Professional Association for Transgender Health (WPATH) standards that Canada generally follows. It is not uncommon for children to start taking puberty blockers at 9 or 10 years old and testosterone or estrogen at 14 or 15.
Age matters because informed consent matters.
While WPATH has dropped all age requirements for hormonal and surgical treatments for gender dysphoria,2 age matters. Age matters because informed consent matters. In Canada, physicians are required to obtain the informed consent of any patient before providing medical treatment – including treatment for minors.3 The Supreme Court defines informed consent as anything a reasonable person in the patient’s position would want to know.4 The central principle is clear – physicians have both an ethical and legal duty to “take reasonable steps, at minimum, to ensure patients understand the information provided to them.”5
Studies indicate that adults patients – much less minor patients – often do not understand the information that doctors present to them.6 Furthermore, patients often have a difficult time identifying their own misunderstandings.7 Doctors have an especially heavy burden to clearly convey information when there may be special or unusual risks that may arise from the procedure and when the procedure is elective, as hormonal and surgical treatments for gender dysphoria are.8 A physician must go so far as to describe “infinitesimally small” risks.9 A physician may not simply describe the probabilities of certain risks arising but must explain the full consequences to the patient should the risk materialize, along with the nature and severity of the potential injuries.10 Hormonal and surgical treatments for gender dysphoria involve many and varied risks described in the previous articles.
If the evidence suggests that physicians are already struggling to provide adequate informed consent for far less complicated procedures to adults, how can physicians provide properly informed disclosure in the far more complex cases of gender reassignment surgery to minors?
Furthermore, with a lack of randomized controlled trials in this field to help inform the consent process, the ability to give fully informed consent to any medical transition treatment is dubious even for adults, much less for minors.
There currently are no age restrictions for receiving puberty blockers, cross-sex hormones, or gender reassignment surgery.
But there currently are no age restrictions for receiving puberty blockers, cross-sex hormones, or gender reassignment surgery either in WPATH’s standards of care or Canadian provincial law or regulation. It is difficult to see how a lack of age requirements for hormonal and surgical treatments is acceptable when far less risky or consequential behaviour has age limitations.
Gender clinics require children and adolescents to sign informed consent forms prior to treatment,11 but do they really understand the consequences and risks associated with these procedures? If a girl starts puberty suppressants and testosterone beginning at age 14 and continuing for a few years, it will almost certainly make her sterile. If she continues down this road to receive surgical procedures such as removing her uterus and ovaries, pregnancy is out of the question. Does a 14-year-old girl understand the decision she is making here?
The trial judge in Bell v Tavistock in the United Kingdom concluded that it was “very doubtful” that 14- or 15-year-olds have such competence and “highly unlikely” that children aged 13 or under have competence for that decision.12 That case centred around the question of whether minors have the capacity to consent to medical or surgical transitioning.
It is impossible for minors to have the capacity to give informed consent to the irreversible effects of medical and surgical transitioning.
In almost every other circumstance in which a minor needs medical care, their parents or guardians consent on behalf of the child. This reflects a common understanding that minors do not have the capacity to consent in the same manner as an adult. However, when it comes to treating gender dysphoria, there is a growing pattern of excluding parents from the entire treatment process if they object to a medical transition.13 This includes courts even forbidding a parent from objecting to his child’s medical transitioning in public and using his child’s birth name and pronouns and throwing him in jail for violating these court orders.14
In summary, we think that it is impossible for minors to have the capacity to give informed consent to the irreversible effects of medical and surgical transitioning. That is why we are campaigning to Let Kids Be and to ban medical and surgical transitioning specifically for minors.
- Justice Education Society, “Youth Age-Based Legal Rights in BC,” accessed March 31, 2023, http://legalrightsforyouth.ca/age-based-legal-rights. ↩︎
- Coleman et al., “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8.” ↩︎
- For a full overview of Canada’s informed consent legislation see, Gerald B Robertson & Ellen I Picard, Legal Liability of Doctors and Hospitals in Canada, 5th ed (Toronto: Thomson Reuters Canada, 2017) at 100-109; 154-204 [Legal Liability of Doctors]. ↩︎
- See, Reibl v Hughes, [1980] 2 SCR 880, 114 DLR (3d) 1, aff’m in Ciarlariello v Schacter, [1993] 2 SCR 119, 100 DLR (4th) 609. ↩︎
- Sarah Birmingham, Christen Rachul & Timothy Caulfield, “Informed Consent and Patient Comprehension: The Law and Evidence” (2013) 7:1 McGill JL & Health 123 at para 5 [Informed Consent and Patient Comprehension]. ↩︎
- BM Stanley, DJ Walters & GJ Maddern, “Informed Consent: How Much is Enough?” (1998) 68 Australian & New Zealand Journal of Surgery 788; Jeff Whittle et al, “Understanding of the Benefits of Coronary Revascularization Procedures Among Patients Who are Offered Such Procedures” (2007) 154 American Heart Journal 662; Allison E Crepeau et al, “Prospective Evaluation of Patient Comprehension of Informed Consent” (2011) 93:19 Journal of Bone & Joint Surgery American Volume 114; Jü JW Wulsow, T Martin Feeley * Sean Tierney, “Beyond Consent: Improving Understanding in Surgical patients” (2012) 203:1 American Journal of Surgery 112; Sonu Pathak et al, “Consent for Gynaecological Procedure: What Do Women Understand and Remember?” (2013) 287 Archives of Gynecology & Obstetrics 59. ↩︎
- Informed Consent and Patient Comprehension, supra note 35 at para 8. ↩︎
- An elective procedure is one that is not medically necessary. See, Philion v Smith, [2008] OJ No 3412. Other examples of elective procedures include cosmetic surgery, sterilization, and even abortion. See Legal Liability of Doctors, supra note 33 at 180-81. ↩︎
- Kitchen v McMullen, 100 NBR (2d) 91, 62 DLR (4th) 481 (NBCA), leave to appeal to SCC refused [1990] 1 SCR viii. ↩︎
- Revell v Chow, 2010 ONCA 353 at para 43. ↩︎
- See, for example, BC Children’s Hospital Gender Clinic, “Information Sheet: Testosterone for Assigned Females with Gender Dysphoria,” December 5, 2022, http://www.bcchildrens.ca/endocrinology-diabetes-site/documents/transtestosterone.pdf; BC Children’s Hospital Gender Clinic, “Information Consent Form: Minor Youth Testosterone for Assigned Females with Gender Dysphoria,” December 14, 2020, http://www.bcchildrens.ca/endocrinology-diabetes-site/documents/transconsentminor-t.pdf; Sick Kids, “Information Form: Testosterone Therapy for Individuals with Gender Dysphoria Assigned Female at Birth,” 2023. ↩︎
- Bell v. Tavistock, [2020] EWHC 3274 ↩︎
- See, for example, the legal case of A.B. v. C.D. and E.F., 2020 BCCA 11 ↩︎
- National Post, “B.C. father arrested, held in jail for repeatedly violating court orders over child’s gender transition therapy,” March 17, 2021, https://nationalpost.com/news/b-c-father-arrested-held-in-jail-for-repeatedly-violating-court-orders-over-childs-gender-transition-therapy ↩︎
Gender-affirming care – the approach of affirming a person’s self-defined gender identity and changing the appearance of the body to align with this identity – is essentially the only response to gender dysphoria. So, this treatment, these puberty blockers, cross-sex hormones, and surgical transitions, must have a solid track record of success, right?
Unfortunately, no. There are no studies that compare the health outcomes of children and adolescents who receive gender-affirming care with those whose gender dysphoria resolved after puberty without medical or surgical intervention. We’ll repeat that. There are no studies that compare the health outcomes of children and adolescents who receive gender-affirming care with those whose gender dysphoria resolved after puberty without medical or surgical intervention.
The reason where there are no studies comparing whether watchful waiting or gender-affirming care is the better response to gender dysphoria is primarily because researchers have considered it unethical to randomly selecting some patients for medical transition and some patients for a wait and see approach.1 Such a random assignment is critically important to determine cause and effect and to generalize results to a broader population. Researchers have devised other ways to design studies to measure the impact of gender-affirming care on patients, but none of them are of high quality or high confidence.2
There are no studies that compare the health outcomes of children and adolescents who receive gender-affirming care with those whose gender dysphoria resolved after puberty without medical or surgical intervention.
In other words, there is no gold-standard evidence that receiving remarkably invasive and irreversible gender-affirming care leads to better outcomes than interventions that actively decrease cross-gender identification or watchfully wait for gender dysphoria to subside.3
In fact, there is lots of evidence that suggests that gender-affirming care is actually harmful.
Let’s start with puberty blockers. Puberty blockers are often compared to hitting the pause button on puberty to allow time for a child to explore their gender identity. But endocrinologist William Malone describes how, after a while, “the [endocrine] system ‘goes to sleep’ and at some point it may not wake up.”4 Abigail Shrier notes, “we wouldn’t consider a drug that stunted your growth in height and weight to be a psychologically neutral intervention – because it isn’t one… and yet the change in height brought on by growth hormones is arguably far less profound than that caused by puberty’s years-long flood of hormones, which transform our bodies into sexual adults.”5 Another concern is that one of the drugs commonly used to block puberty, Lupron, is the same drug was used to chemically castrate sex offenders. It is approved to treat symptoms of prostate cancer, endometriosis, and precocious puberty but is used “off-label” in a medical transition.
“We wouldn’t consider a drug that stunted your growth in height and weight to be a psychologically neutral intervention – because it isn’t…”
Abigail Shrier
Common side effects of puberty blockers are redness/burning/stinging/pain/bruising at the injection site, hot flashes, increased sweating, night sweats, tiredness, headache, upset stomach, nausea, diarrhea, constipation, stomach pain, breast swelling or tenderness, acne, joint/muscle aches or pain, trouble sleeping (insomnia), reduced sexual interest, vaginal discomfort/dryness/itching/discharge, vaginal bleeding, swelling of the ankles/feet, increased urination at night, dizziness, breakthrough bleeding in a female child during the first 2 months of leuprolide treatment, weakness, chills, clammy skin, skin redness, itching or scaling, testicle pain, impotence, depression, increased growth of facial hair, and memory problems.6
And then there is cross-sex hormones. The risks from cross-sex hormones are even more serious, and include venous thromboembolism (blood clots), hyperkalemia (high potassium), hypertriglyceridemia (high level of fats in blood), polycythemia (high red blood cell count), hyperprolactinemia (high prolactin hormone levels), decreased HCL cholesterol and increased LDL cholesterol, hypertension (high blood pressure), cardiovascular disease, cerebrovascular disease, meningioma (brain tumor), polyuria (excessive urine production), dehydration, cholelithiasis (gallstones), type 2 diabetes, low bone mass, osteoporosis, weight gain, acne, sleep apnea, androgenic alopecia (hair loss), erectile dysfunction, and infertility.7
And this is just the list of possible effects of hormonal treatment. Surgical interventions can bring a host of new adverse effects, depending on the type of surgery. For example, there are numerous reports of hair painfully growing within the neo-vaginal lining follow a vaginoplasty, urination complications following a phalloplasty, and even fatal sepsis following a mastectomy. Most forms of bottoms surgery are guaranteed to lead to infertility: how can someone father a child if their testicles have been removed or conceive a baby of their uterus is gone?
Those are the risks for what is supposed to be gender-affirming care. But are there any benefits?
While some studies document improved mental health outcomes after hormonal or surgical interventions,8 these studies only report on short-term outcomes. Much more valuable studies, known as longitudinal studies, track outcomes over long periods of time. The best longitudinal study, headed by Swedish researcher Cecilia Dhejne, found that health outcomes deteriorate just one year after undergoing a surgical transition. By the fifth year after surgery, patients had poorer outcomes in seven of eight measured categories: mental health, vitality, bodily pain, social function, emotional functioning, physical functioning, and general health.9
“Gender-affirming care” is a misnomer.
It’s not caring at all.
These are only some of the harms of medical gender transitioning. And this is why “gender-affirming care” is a misnomer. It’s not caring at all. It ignores our biological identity as a male or a female, and so perhaps it isn’t all that surprising that there are all of these negative effects of medical or surgical transitioning.
So, what counts as success when treating gender dysphoria? All sides in this debate should agree that, at a minimum, the loss of fertility and increased risk of a host of serious medical conditions, are not signs of success. Yet, these are the results of medical transitioning far too often.
Defining success as improved life satisfaction and decreased risk of suicidality and self-harm is a good step in the right direction, but even on this score, the long-term data on these measures of success do not favour medical transitioning.
- See Michelle A Cretella, “Gender Dysphoria in Children and Suppression of Debate” 21, no. 2 (2016). ↩︎
- See Society for Evidence-Based Gender Medicine, “International Perspectives on Evidence-Based Treatment for Gender-Dysphoric Youth Conference,” October 10-11, 2023, New York ↩︎
- See Yarhouse, Understanding Gender Dysphoria, 102–3. for a description of these approaches ↩︎
- Shrier, Irreversible Damage, 165. ↩︎
- Shrier, 164. ↩︎
- Lupron, (October 12, 2021), RxList, https://www.rxlist.com/lupron-drug.htm ↩︎
- Talal Alzahrani et al., “Cardiovascular Disease Risk Factors and Myocardial Infarction in the Transgender Population,” Circulation: Cardiovascular Quality and Outcomes 12, no. 4 (April 2019): e005597, https://doi.org/10.1161/CIRCOUTCOMES.119.005597; Michael S. Irwig, “Cardiovascular Health in Transgender People,” Reviews in Endocrine and Metabolic Disorders 19, no. 3 (September 1, 2018): 243–51, https://doi.org/10.1007/s11154-018-9454-3; Stephen M. Rosenthal, “Challenges in the Care of Transgender and Gender-Diverse Youth: An Endocrinologist’s View,” Nature Reviews Endocrinology 17, no. 10 (October 2021): 581–91, https://doi.org/10.1038/s41574-021-00535-9; Silvano Bertelloni et al., “Final Height, Gonadal Function and Bone Mineral Density of Adolescent Males with Central Precocious Puberty after Therapy with Gonadotropin-Releasing Hormone Analogues,” European Journal of Pediatrics 159, no. 5 (April 1, 2000): 369–74, https://doi.org/10.1007/s004310051289; Ana Antun et al., “Longitudinal Changes in Hematologic Parameters Among Transgender People Receiving Hormone Therapy,” Journal of the Endocrine Society 4, no. 11 (November 1, 2020): bvaa119, https://doi.org/10.1210/jendso/bvaa119; Hayley Braun et al., “Moderate-to-Severe Acne and Mental Health Symptoms in Transmasculine Persons Who Have Received Testosterone,” JAMA Dermatology 157, no. 3 (March 1, 2021): 344–46, https://doi.org/10.1001/jamadermatol.2020.5353; Mauro E. Kerckhof et al., “Prevalence of Sexual Dysfunctions in Transgender Persons: Results from the ENIGI Follow-Up Study,” The Journal of Sexual Medicine 16, no. 12 (December 1, 2019): 2018–29, https://doi.org/10.1016/j.jsxm.2019.09.003; Spyridoula Maraka et al., “Sex Steroids and Cardiovascular Outcomes in Transgender Individuals: A Systematic Review and Meta-Analysis,” The Journal of Clinical Endocrinology & Metabolism 102, no. 11 (November 1, 2017): 3914–23, https://doi.org/10.1210/jc.2017-01643; M. Kyinn et al., “Weight Gain and Obesity Rates in Transgender and Gender-Diverse Adults before and during Hormone Therapy,” International Journal of Obesity 45, no. 12 (December 2021): 2562–69, https://doi.org/10.1038/s41366-021-00935-x; Sebastian E E Schagen et al., “Bone Development in Transgender Adolescents Treated With GnRH Analogues and Subsequent Gender-Affirming Hormones,” The Journal of Clinical Endocrinology & Metabolism 105, no. 12 (December 1, 2020): e4252–63, https://doi.org/10.1210/clinem/dgaa604; Daniel Klink et al., “Bone Mass in Young Adulthood Following Gonadotropin-Releasing Hormone Analog Treatment and Cross-Sex Hormone Treatment in Adolescents With Gender Dysphoria,” The Journal of Clinical Endocrinology & Metabolism 100, no. 2 (February 1, 2015): E270–75, https://doi.org/10.1210/jc.2014-2439; Magdalena Dobrolińska et al., “Bone Mineral Density in Transgender Individuals After Gonadectomy and Long-Term Gender-Affirming Hormonal Treatment,” The Journal of Sexual Medicine 16, no. 9 (September 1, 2019): 1469–77, https://doi.org/10.1016/j.jsxm.2019.06.006; Darios Getahun et al., “Cross-Sex Hormones and Acute Cardiovascular Events in Transgender Persons,” Annals of Internal Medicine 169, no. 4 (August 21, 2018): 205–13, https://doi.org/10.7326/M17-2785; Mariska C. Vlot et al., “Effect of Pubertal Suppression and Cross-Sex Hormone Therapy on Bone Turnover Markers and Bone Mineral Apparent Density (BMAD) in Transgender Adolescents,” Bone 95 (February 1, 2017): 11–19, https://doi.org/10.1016/j.bone.2016.11.008; Iris E. Stoffers, Martine C. de Vries, and Sabine E. Hannema, “Physical Changes, Laboratory Parameters, and Bone Mineral Density During Testosterone Treatment in Adolescents with Gender Dysphoria,” The Journal of Sexual Medicine 16, no. 9 (September 1, 2019): 1459–68, https://doi.org/10.1016/j.jsxm.2019.06.014; Michael Biggs, “Revisiting the Effect of GnRH Analogue Treatment on Bone Mineral Density in Young Adolescents with Gender Dysphoria,” Journal of Pediatric Endocrinology and Metabolism 34, no. 7 (July 1, 2021): 937–39, https://doi.org/10.1515/jpem-2021-0180; Rafael Delgado-Ruiz, Patricia Swanson, and Georgios Romanos, “Systematic Review of the Long-Term Effects of Transgender Hormone Therapy on Bone Markers and Bone Mineral Density and Their Potential Effects in Implant Therapy,” Journal of Clinical Medicine 8, no. 6 (June 2019): 784, https://doi.org/10.3390/jcm8060784; Tobin Joseph, Joanna Ting, and Gary Butler, “The Effect of GnRH Analogue Treatment on Bone Mineral Density in Young Adolescents with Gender Dysphoria: Findings from a Large National Cohort,” Journal of Pediatric Endocrinology and Metabolism 32, no. 10 (October 1, 2019): 1077–81, https://doi.org/10.1515/jpem-2019-0046; Kyinn et al., “Weight Gain and Obesity Rates in Transgender and Gender-Diverse Adults before and during Hormone Therapy”; Noreen Islam et al., “Is There a Link Between Hormone Use and Diabetes Incidence in Transgender People? Data From the STRONG Cohort,” The Journal of Clinical Endocrinology & Metabolism 107, no. 4 (April 1, 2022): e1549–57, https://doi.org/10.1210/clinem/dgab832. ↩︎
- See Coleman et al., “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8.” for a sample of studies ↩︎
- Cecilia Dhejne et al., “Long-Term Follow-Up of Transsexual Persons Undergoing Sex Reassignment Surgery: Cohort Study in Sweden,” PLOS ONE 6, no. 2 (February 22, 2011): e16885, https://doi.org/10.1371/journal.pone.0016885. ↩︎
Most people’s gender identity – their self-perception of being male or female – aligns with their biological sex. According to the 2021 census, 99.7% of Canadians aged 15 years and older affirm that their internalized gender identity matches their biological sex (Statistics Canada). A small minority of people – the remaining 0.33% of Canadians – experience gender dysphoria.
Gender dysphoria is a condition in which a person’s gender identity does not match their sex (see note). For example, someone who is a biological female may feel that she is, or should be, male. Gender dysphoria, a psychological phenomenon, is not to be confused with biological disorders of sexual development, which are even more rare.
While there is no single, generally accepted cause for gender dysphoria, there are discernible trends among children and adolescents with gender dysphoria. Among children who exhibit gender dysphoria prior to puberty, approximately 80% will “desist” or out-grow this dysphoria by adulthood.* However, the number of post-pubescent adolescents – teenage girls in particular – with gender dysphoria has skyrocketed in western countries like Canada, the United States, and the United Kingdom in recent years. Researchers have called this phenomenon rapid-onset gender dysphoria and some suggest that it is a social contagion.**
Among children who exhibit gender dysphoria prior to puberty, approximately 80% will “desist” or out-grow this dysphoria by adulthood.
The current Canadian approach to treating gender dysphoria is called, euphemistically, gender-affirming care. This approach to care is described in the World Professional Association on Transgender Health (WPATH)’s Standards of Care. Canadian provinces generally follow these WPATH standards, albeit with significant differences between provinces. Regulatory colleges recommend or require this approach. Under this approach, when a child or adolescent reaches out to a health practitioner about gender dysphoria, the practitioner affirms the patient’s self-perceived gender identity and seeks to change the patient’s body to appear more like the desired sex.
In other words, unlike in other areas of medicine, gender clinicians typically agree with patients’ (or, in the case of young children, their parents’) self-diagnosis of gender dysphoria and refer for treatment on the basis of this self-diagnosis. The clinician doesn’t perform any tests to diagnose gender dysphoria. The clinician can’t encourage a child to think of themselves or act in a way that corresponds with their birth sex – that’s illegal under Canada’s ban on conversion therapy. Under the paradigm of gender-affirming care, there is only one acceptable treatment direction: onward to a medical and/or surgical transition.
According to WPATH’s standards, medical practitioners should only proceed to gender-affirming medical and surgical treatment for minors if:
- Gender dysphoria is marked and sustained over time;
- The diagnostic criteria of gender dysphoria are met (as per International Classification of Diseases 11)11;
- The patient demonstrates the emotional and cognitive maturity required to provide informed consent;
- Mental health concerns (if any) have been addressed;
- The patient has been informed of the effects of treatment on reproduction;
- The patient has reached Tanner stage 2 of puberty (the beginning of the physical stages of puberty) for puberty blockers and cross-sex hormones; and
- The patient has received at least 12 months of gender-affirming hormone therapy (before gender reassignment surgery can be performed).***
The fundamental problem with gender-affirming care is that it misdiagnoses the problem. Gender dysphoria is not a problem of the body. While gender identity and gender expression can change over the course of someone’s lifetime, biological sex cannot change.
“The fundamental problem with gender-affirming care is that it misdiagnoses the problem.”
True, hormone injections can trigger the development of secondary sex characteristics (e.g. facial hair, lower voice, or an Adam’s apple). And surgical procedures can remove or create imitations of reproductive organs. However, hormones and surgeries cannot change the fundamental sexual organization of the human body as male or female.
A person’s sex is objectively determined by the organization of their body for a specific reproductive role – to produce sperm cells (male gametes) or egg cells (female gametes), as evidenced by the person’s sex chromosomes, naturally occurring sex hormones, and internal and external genitalia. Aside from extremely rare genetic disorders, each cell in a person’s body has either an XY chromosome (male) or an XX chromosome (female). In short, while these gender transition surgeries are often called “sex change surgeries,” such a term is a misnomer because it’s impossible to change your biological sex.
Gender-affirming care assumes that the fundamental problem is that a person is born into the wrong body. By getting the problem wrong, it also gets the solution wrong. Its misguided solution to gender dysphoria is to radically reshape the body, at great cost to physical health (more on that in a future post).
“The solution is not to radically reshape the body through drugs, hormones, and surgery. The solution is to help someone accept and love their natural body. ”
The problem of gender dysphoria does not lie with the body. It lies with the mind. Those who experience gender dysphoria have nothing wrong with their body. Rather, they have difficulty identifying with or accepting their body. That is a real and very difficult struggle. But the solution is not to radically reshape the body through drugs, hormones, and surgery. The solution is to help someone accept and love their natural body.
In a review of Johns Hopkins University’s “sex change” clinic, former director Dr. Paul McHugh states that “in a thousand subtle ways, the re-assignee has the bitter experience that he is not — and never will be — a real girl but is, at best, a convincing simulated female. Such an adjustment cannot compensate for the tragedy of having lost all chance to be male, and of having in the final analysis, no way to be really female.”1
Dr. Sander Breiner agrees, explaining that she and her colleagues at Michigan’s Wayne State University had to tell the surgeons that “the disturbed body image was not an organic [problem] at all, but was strictly a psychological problem. It could not be solved by organic manipulation (surgery, hormones).”2
It is common today for people to speak of being a woman trapped in a man’s body or a man trapped in a woman’s body. But, as Toronto psychiatrist Dr. Joseph Berger explains, “scientifically, there is no such thing.”3
Note:
There are a variety of words used to describe this phenomenon. ARPA Canada prefers the term “gender dysphoria,” found in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders V. The International Classification of diseases uses “gender incongruence,” WPATH prefers the term “transgender and gender diverse people,” while the vernacular defaults to the descriptor “transgender.”
Sources:
* See for example Thomas D. Steensma and Peggy T. Cohen-Kettenis, “A Critical Commentary on ‘A Critical Commentary on Follow-up Studies and “Desistence” Theories about Transgender and Gender Non-Conforming Children,’” International Journal of Transgenderism 19, no. 2 (April 3, 2018): 225–30; Thomas Steensma and Peggy Cohen-Kettenis, “Gender Transitioning before Puberty?,” Archives of Sexual Behavior 40 (March 1, 2011): 649–50; Thomas D. Steensma et al., “Desisting and Persisting Gender Dysphoria after Childhood: A Qualitative Follow-up Study,” Clinical Child Psychology and Psychiatry 16, no. 4 (October 1, 2011): 499–516; Kelley D. Drummond et al., “A Follow-up Study of Girls with Gender Identity Disorder,” Developmental Psychology 44 (2008): 34–45; Madeleine S. C. Wallien and Peggy T. Cohen-Kettenis, “Psychosexual Outcome of Gender-Dysphoric Children,” Journal of the American Academy of Child and Adolescent Psychiatry 47, no. 12 (Dec 2008): 1413–23; Susan J. Bradley and Kenneth J. Zucker, “Gender Identity Disorder and Psychosexual Problems in Children and Adolescents,” The Canadian Journal of Psychiatry 35, no. 6 (August 1, 1990): 477–86; Jiska Ristori and Thomas D. Steensma, “Gender Dysphoria in Childhood,” International Review of Psychiatry 28, no. 1 (2016): 13–20; Devita Singh, Susan J. Bradley, and Kenneth J. Zucker, “A Follow-Up Study of Boys With Gender Identity Disorder,” Frontiers in Psychiatry 12 (2021).
** Lisa Littman, “Parent Reports of Adolescents and Young Adults Perceived to Show Signs of a Rapid Onset of Gender Dysphoria,” PLOS ONE 13, no. 8 (August 16, 2018): e0202330; Abigail Shrier, Irreversible Damage (New Jersey: Regnery Publishing, 2020).
*** Coleman et al., “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8,” 18.
1. Dr. Paul McHugh is Distinguished Service Professor of Psychiatry at Johns Hopkins University. In 2004, Dr. McHugh published an article explaining the scientific reasons for rejecting sex change procedures. After describing the great deal of damage he witnessed from sex-reassignment, he concluded, “we psychiatrists have been distracted from studying the causes and natures of their mental misdirections by preparing them… for a life in the other sex. We have wasted scientific and technical resources and damaged our professional credibility by collaborating with madness rather than trying to study, cure, and ultimately prevent it.” Paul R. McHugh, “Surgical Sex: Why We Stopped Doing Sex Change Operations” (Nov. 2004) First Things.
2. Sander Breiner, M.D., “Transsexuality Explained,” National Association for Research and Therapy of Homosexuality, n.d., accessed March 26, 2015. Dr. Breiner also explained that “[T]he significance of the psychological difficulty should not be minimized by a patient’s seeming success, socially and professionally, in other areas”.
3. Written testimony of Dr. Joseph Berger to the House of Commons Standing Committee on Justice and Human Rights, regarding Bill C-279.
In the first policy of its kind in Canada, Alberta will be limiting medical transitioning for minors.
Until now, there has been no legislation, regulation, or official policy about when minors can access puberty blockers, cross sex hormones, or transition-related surgery. Many countries around the world (such as Finland, Sweden, the United Kingdom, and France) as well as 22 American states have already limited medical transitioning for minors. Canadian provinces held doggedly to the deeply flawed World Professional Association on Transgender Health (WPATH)’s standards of care, which list no age restriction for medical transitioning.
That changed when Alberta Premier Danielle Smith made a suite of announcements relating to transgender policy.
The most important policy change is that puberty blockers and cross-sex hormones will be banned for those aged 15 and under. For youth aged 16 or 17, parental, physician, and psychologist approval will be required to begin a medical transition.
There is no comprehensive data available on the number of minors receiving puberty blockers and cross-sex hormones across Canada. But considering that most puberty blockers are prescribed near the onset of puberty, this policy will likely prevent many children from starting on the medical transition conveyor belt at an early age and going on to receive cross-sex hormones and surgery.
This is good for children. There is little evidence on the long-term safety of puberty blockers, and there are many documented risk factors associated with cross-sex hormones, including blood clots, heart disease, cerebrovascular disease, brain tumors, and osteoporosis.
Top surgeries (mastectomies) and bottom surgeries (phalloplasties, vaginoplasties, and metoidioplasties) will be banned for minors aged 17 and under in Alberta. According to information released by the Canadian Institute for Health Information (CIHI), while there are very few bottom surgeries performed on minors in Canada, there are dozens of minors having mastectomies every year.
The message from the Alberta premier is clear: children do not have the capacity to make these profound decisions about their bodies.
Regardless of how many damaging prescriptions or procedures these new rules prevent, the message from the Alberta premier is clear: children do not have the capacity to make these profound decisions about their bodies. The Alberta health system will no longer be party to these procedures for minors aged 15 years and below.
Premier Smith applied the same logic to school settings. Following the lead of New Brunswick and Saskatchewan, Alberta will require parental notification and consent if a child aged 15 or under wishes to change their name or pronouns at school. For minors aged 16 or 17, parental notification for name or pronoun changes will still be required. Seventy-eight percent of Canadians and 88% of Albertans favour this policy change, as measured in an Angus Reid poll last July.
Alberta will also require teachers to notify parents before giving formal instruction on gender, sexual orientation or human sexuality in the classroom. Parents must actively opt into their children receiving such instruction. This is a significant change from the previous policy, where teaching about sexual orientation and gender identity (SOGI 123) was adopted by school districts across the province and embedded throughout the curriculum.
Finally, the Alberta government committed to work with sporting organizations to ensure that biological women and girls have the choice to compete in athletic competitions in a women-only division without any trans-identifying males. This policy recognizes that men and women, boys and girls have fundamentally different bodies with different performance capabilities.
These developments – particularly the age restrictions for medical transitioning – are enormous.
These developments – particularly the age restrictions for medical transitioning – are enormous. Countries and states around the world that have taken time to review the evidence in favour of medical transitioning have found it lacking and, in the interest of protecting the health of children, have limited medical transitioning for minors. It is not only appropriate but morally responsible of Alberta to limit these procedures. We call on other Canadian provinces to follow Alberta’s lead and end medical transitioning for minors.
Childhood is a precious time that should be protected. We need to let kids be – let them grow and develop naturally. Children who suffer from gender dysphoria have an identity struggle. But there is nothing medically wrong with their bodies, and it is entirely inappropriate to medically or surgically alter children’s bodies to solve an identity crisis. In fact, over 80% of cases of pre-pubescent gender dysphoria go away after puberty. Medical transitioning not only is unnecessary, but harmful. Instead, we simply need to let kids be.